The Damaging Effects of Autonomic Dysfunction After a Concussion
Our bodies have an automatic system that controls hundreds of involuntary processes, like breathing, heart rate, digestion, sexual response, and metabolism. This ancient system, called the autonomic nervous system (or ANS for short) has two parts: the sympathetic or “fight-or-flight” pathway, and the parasympathetic or “rest-and-digest” pathway.
Traumatic brain injury and concussions, like many serious injuries, causes the ANS to ramp up the protective “fight or flight” reaction. The body rushes nutrients to the injured area, fires up the immune system to deal with injured tissues, keep us on high alert, blunts our pain response, sends our blood pressure and heart rate soaring, makes our breathing rapid and shallow, and pours glucose into the body to enable us to flee if the threat comes back. Functions deemed not essential for immediate survival are drastically reduced: digestion, sexual function, and sleep are among the first victims.
The body cannot stay in this state for very long before our health starts to suffer. Even though the system is designed to return itself to balance, sometimes injuries overwhelm its ability to turn off the “fight or flight” reaction. Concussions frequently throw the ANS into disarray, causing a host of seemingly mysterious and debilitating symptoms. I call this imbalanced state “injury shock”.
Sometimes this imbalance becomes chronic. This state of perpetual stress can have potentially catastrophic health consequences. Chronic “autonomic dysfunction” is one of the most common, persistent, and disabling consequences of concussions.
For over a hundred years, osteopathic physicians have been designing and refining effective techniques to address autonomic dysfunction and restore the autonomic nervous system to balance. With our reverence for the vagus nerve - the major nerve of the ANS - along with the diaphragm, ribs and the breath, we have numerous techniques for healing ANS problems.
“Why Can’t I Calm Down?”
It’s very common for people who have had a concussion or TBI to have an overactive sympathetic response. It is not your imagination or because you are weak that you can’t sleep, have trouble eating, are irritable and angry with your family, have heart palpitations, or are depressed. It’s common and there are sound physiological reasons for it. Many times there are structural causes of autonomic problems, which you can read about below. By addressing restrictions in the ribs and the diaphragm, for example, osteopathic physicians can help restore healthy breathing. We also can take pressure off compressed nerve bundles along the spine whose irritation makes people feel like they are still under attack.
How You Can Treat Acute Injury Shock
There are some things you can do yourself to calm your agitated nervous system. Practices like yoga, meditation and swimming (because of its breathing requirements) are excellent at helping the ANS put itself back into balance. I talk about this in more detail in Healing Pain and Injury.
•MEDITATION with a focus on the breath is an excellent way to help restore natural breathing patterns. If you don’t know how to meditate, there are many helpful classes and APPS available to help you.
•YOGA is masterful at helping the diaphragm relax and in restoring normal breathing patterns. It also can help restore the calming parasympathetic nervous system.
• SWIMMING is helpful because of its ability to restore a normal breathing pattern. I advise my patients to swim with a mask and snorkel if they have a sore neck.
•WALKING IN NATURE can be very soothing as well.
•THE SIMPLE ACT OF RHYTHMIC BREATHING can reset the autonomic nervous system. Dr. Andrew Weil has developed a practice called “4-7-8” breathing in which you inhale for a count of 4, hold your breath for a count of 7, and exhale for a count of 8 (imagining you are exhaling through a straw can help). It is recommended you try this for 4 breaths, twice a day, to start.
•There are APPS available that help the heart regain its normal rhythm, known as Heart Rate Variability. HEART MATH is probably the best known, but there are many others.
•There are APPS available that help the heart regain its normal rhythm, known as Heart Rate Variability. HEART MATH is probably the best known, but there are many others.
What To Do When You Need Help To Treat Injury Shock
Autonomic problems sometimes need the help of a skilled practitioner. Sometimes,all the yoga, swimming, and meditation in the world is not enough. If a structural problem is contributing to your stress, an osteopathic practitioner or skilled manual medicine practitioner trained in treating the nervous system can help.
Here are some of the structural problems that can contribute to ongoing Injury Shock:
Chest and Rib Injuries
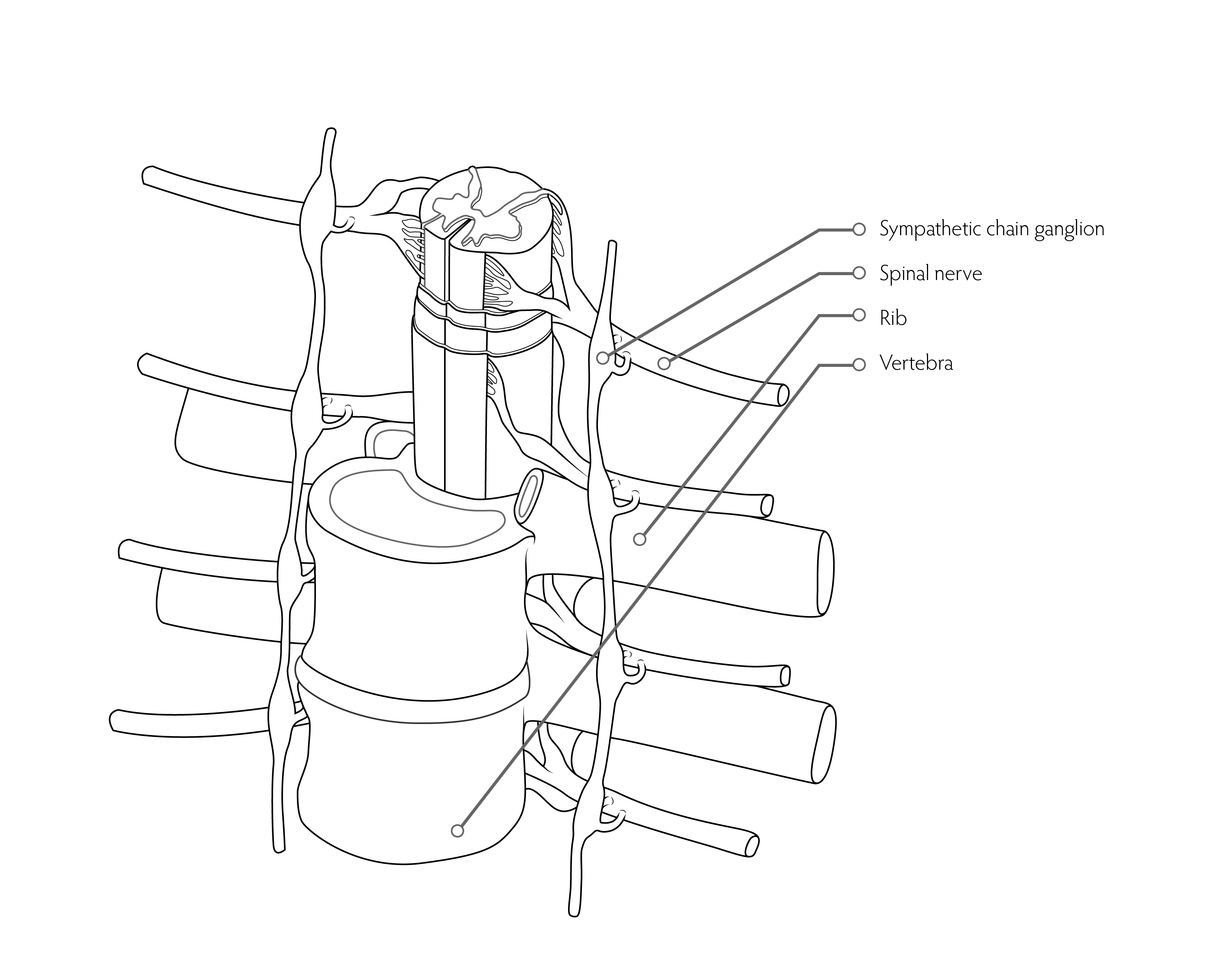
If you have a chest injury - for example, if you hit the seat belt very hard - the rib heads can get compressed into the spine where the “hubs” or “ganglion” of the sympathetic nervous system live. The SNS is mechanically stimulated every time you breathe, keeping the heart beating too fast. Sometimes, just freeing up the ribs can calm the SNS down.
Restricted Diaphragm

2. Who hasn’t “gasped” when faced with danger or injury? Sometimes we are so surprised by an accident that we involuntarily gasp and lock up the diaphragm. The sympathetic nervous system cannot calm down if you constantly are taking shallow breaths. Working to release the diaphragm from its post-accident spasm can help calm the SNS down. And since the heart’s covering (the pericardium) is attached to the diaphragm, a shallow moving diaphragm can literally cause the heart to beat faster, revving up the fight or flight response.
Unhappy Vagus Nerve
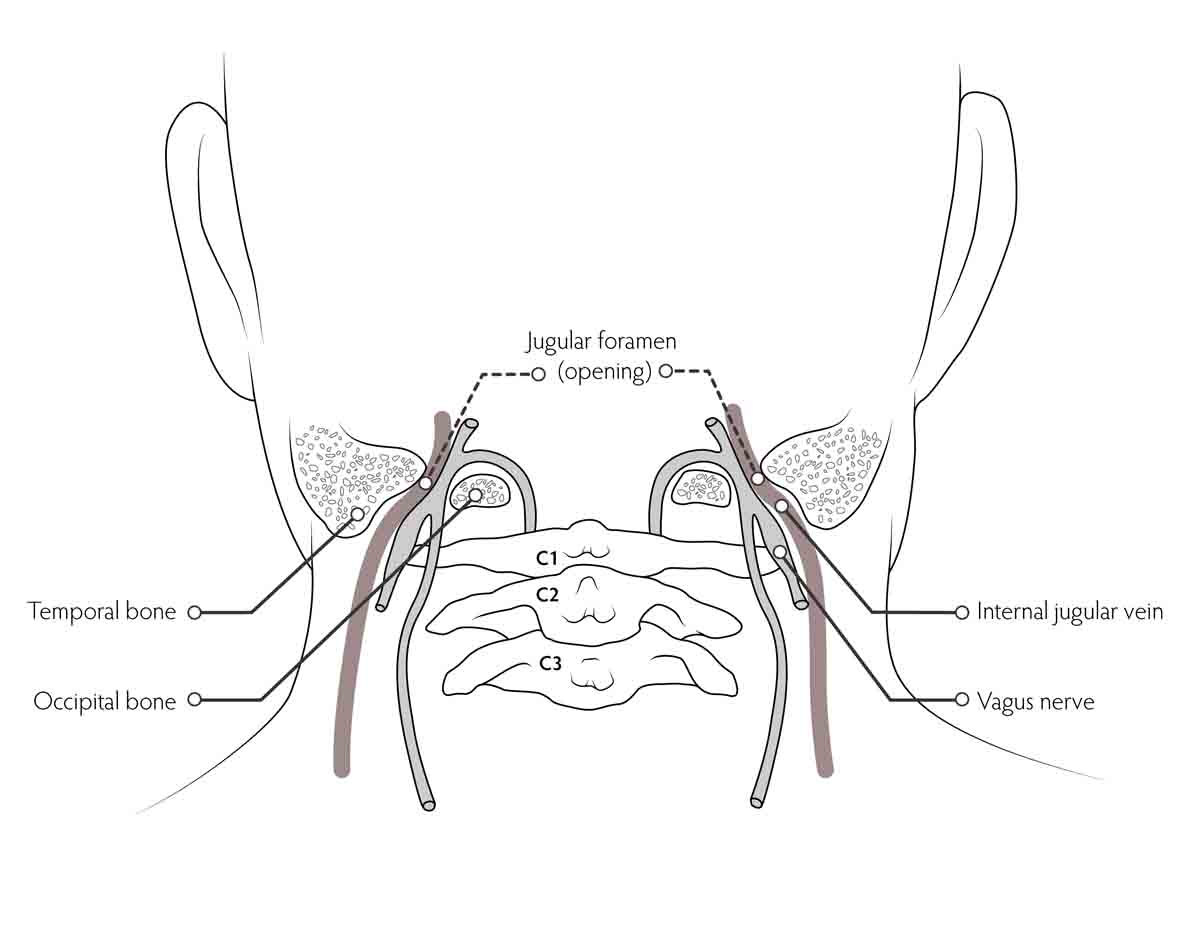
3. The master of the calming parasympathetic nervous system, the vagus nerve, exits the back of the skull through two openings called the jugular foramen (so called because the vagus nerve shares this opening with the jugular veins). Sometimes the opening gets pinched because by the upper vertebra of the neck. If the vagus nerve doesn’t have the juice to help the nervous system calm down, the ANS will not be able to return to balance.
Central Autonomic Network Problems
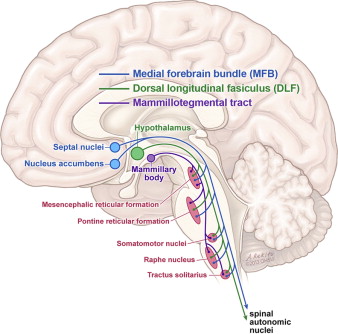
4. Many structures deep within the brain help govern the ANS response to injury. Sometimes those structures are injured or impaired during a concussion. Helping theses structures heal requires a skilled and experienced practitioner of cranial osteopathic manual medicine. It is definitely not for the inexperienced practitioner.
Neck Problems

Frequently the same forces that injure the brain act like a karate chop to the neck. The neck is the superhighway through which the autonomic nervous system signals have to pass. Neck injury can impact autonomic function, and frequently requires a skilled practitioner to help it heal.
Autonomic Dizziness

Dizziness and vertigo can have many causes after a concussion, but sometimes it’s an autonomic problem. Dr.John Leddy of the University of New York at Buffalo has pioneered the development of a protocol for slowly restoring ANS function in athletes with autonomic dizziness known as the Buffalo Protocol. If you have problems with exercise intolerance, find a practitioner who is familiar with the Buffalo Protocol to help you get back in the game.
Symptoms of acute Injury shock
The Long Term Effects of Injury Shock
Evidence is emerging that autonomic dysfunction can persist for years after a concussion has seemingly resolved. Given the wide-ranging influence of the ANS over the heart and cerebral circulation and the mounting evidence that the ANS is a critical factor in depression and PTSD, I believe we will find that ANS dysfunction plays a key role in devastating chronic conditions such as stroke, heart disease, suicide and depression.
In fact, researchers are now “mining” health care data to find out what happens to head injury patients many years later. This information is available in countries that (unlike the United States) have national health care systems. What we have learned is absolutely shocking. Concussions have been linked to:
•Increased incidence of stroke
•increased incidence of myocardial dysfunction
•Increased incidence of suicide
•Increased risk of premature death from all causes
•Increased risk of poor long-term life outcomes for children